Cancer: Major Good News on Immunotherapy
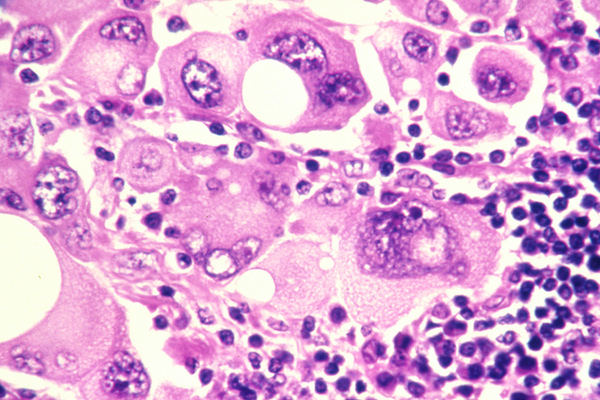
Melanoma cells. National Cancer Institute, public domain.
A mouse study at Stanford University Medical Center that will almost certainly improve cancer treatment in people was published January 31, 2018, in Science Translational Medicine. A headline that 97% of the mice were cured of lymphoma is true, but only part of the story. This experimental treatment may work for many kinds of cancer, not only lymphoma. At least in mice, it eliminated the specific cancer in one tumor anywhere the body, including metastases.
Most of the mainstream press skipped this news, probably because many drugs that work in mice fail to help people. But here the issue isn't whether these drugs work in people, but whether this strategy can be made to work - which is much more likely. And this study will help to advance cancer research in many ways. The daily press must make snap judgments, and mostly missed a major advance of 2018.
Toward Simpler and Better Immunotherapy
Cancer immunotherapy (treating cancer by improving the response of the body's immune system) has been much in the news, especially CAR T, which is now approved - as modern immunotherapies can treat some cancers when standard methods have failed. The recently reported study tested an immunotherapy that is much simpler, almost certainly safer, and likely effective against many kinds of cancer (though we don't know yet, pending human trials). And it could be affordable to everyone, if profiteering doesn't interfere.
The human immune system normally keeps cancer under control, which is why most people don't get cancer despite having trillions of cells that could possibly become cancerous. Successful tumors have usually evolved ways to inactivate the immune system's T-cells, which mobilize the body's defenses against cancer. The researchers believed that two different steps together could restore the T-cells, so the new experimental treatment used a combination of two drugs. Different combinations were tested in mice in preliminary studies, and the best one was chosen.
In the main trials, mice were injected with lymphoma cells in two different parts of the body. When tumors formed, very low doses of the drugs were injected into just one of the tumors. There was no need to treat the other tumor. The doses were low so that the drugs would only act inside that one tumor (instead of treating the T-cells in the whole body, which could cause dangerous side effects). And the T-cells that had infiltrated that tumor are those naturally targeted to that specific cancer - exactly the ones you want to re-activate. The treated T-cells eliminated the tumor - and also the other, untreated tumor of the same cancer. It is likely to eliminate metastases as well - including those that are inoperable, or currently too small to detect. The treatment eliminated both tumors in 87 out of 90 mice; the other three needed a second treatment, which did eliminate the cancer.
Another trial tested the same treatment with breast cancers that had developed spontaneously (in mice genetically engineered to get them), as these might be harder to treat than cancers that were implanted. The treatment worked for these cancers as well.
Both drugs used in the mouse tests have already been accepted for investigational use in human clinical trials, so they have passed basic safety requirements. The very small doses used to treat just one tumor provide more reassurance on safety. This treatment is very targeted to only one kind of cancer, the one in the tumor being treated.
Stanford is now planning a human trial with 15 lymphoma patients. But the researchers also found similar results in mice with breast cancer, colon cancer, and melanoma, and suspect that the treatment may work for most cancers.
Comment
(1) Spontaneous remission. This study might help researchers understand why cancers (very rarely) cure themselves with no treatment. No one knows why this occurs. Could a process similar to that induced in the mice sometimes happen without treatment? Understanding spontaneous remission might lead to new ways to induce it.
(2) Experimental treatments. The pros, cons, and rules of patient access to experimental treatment deserve a separate article. But from our experience publishing AIDS Treatment News for 20 years, three considerations come to mind: (a) Consider conventional treatment first - and note that delaying experimental treatment can give you more news about whether and how to use it. But on the other hand, the current medical-research system was not designed for speed or efficiency, and wastes years in business and regulatory processing and status competition, in addition to the time required for scientific research. (b) Doctors differ greatly in their willingness to try something new - but it helps much if patients have studied their options, know what they want, and ask for it. They might also need another doctor. (c) There are many practical obstacles, and it is best to be in touch with others and work as a community when possible. One place to start is a list of patient communities at e-Patient Dave (http://www.epatientdave.com/communities/). Also, there is a controversial "right to try" movement.
(3) Drug pricing. For the mice, 4 micrograms of one drug and 50 micrograms of the other were administered, repeated 3 times. So even if the drugs cost $1000 a gram to produce (unlikely), the drug cost to treat a mouse would be about 16 cents ($0.16) for the whole treatment course - showing plenty of room for profit without depriving people of access.
The best human dose is unknown, and will presumably be larger; but since only one tumor is being treated, not the whole body, the ratio of human to mouse doses may be much less than the standard dose conversions for whole-body treatment (usually based on body surface area, not body weight).
But in a very unequal world, the usual drug pricing at what the market will bear will set prices for the rich, excluding most people entirely unless governments pay. For example, CAR T cancer treatment, a complex and difficult procedure, can cost $475,000 per patient today and is expected to increase for new versions, pricing treatment and commercial insurance out of reach for most people. Since governments represent the money, people will need to organize (as they did in AIDS) to insist that public interest has some role in access to lifesaving drugs. There must be a middle way that pays for research without blocking access. Or the new generations of cancer treatments will be reserved for the rich, or superstars who can crowdfund their medical care - or those who travel to international cancer havens that will join the tax havens of today.
For More Information
- For non-specialists, the best source for more information is Cancer ‘vaccine’ eliminates tumors in mice, published by Stanford Medicine News Center, 2018-01-31. It is the most authoritative news report, understandable by medical professionals and the interested public.
- The original research paper, Eradication of spontaneous malignancy by local immunotherapy, 2018-01-31, is written for scientists and physicians familiar with cancer immunotherapy. The full text is no longer publicly accessible without a paywall. Sometimes a librarian can get it for you; otherwise you can order a copy of that issue of Science for $15, or get one day of online access to the article for $30.
- Also note Local immunotherapy shrinks tumors near and far, Genetic Engineering News 2018-02-01.
- For more information on the science behind this trial, do a Google or other search for:
Anti-OX40 "TLR9 Agonist"
(which are names of the drug treatments used). - You can do the same search on Twitter - or search for Immunotherapy, or whatever you want - to see what people are talking about right now. (If you don't have a Twitter account, you can use our search box at www.twitter.com/agetreatment, near the top of the page.)

This work is licensed under a Creative Commons Attribution 4.0 International License.